Impact COVID-19 on non-COVID-19 Care at University Hospital Brussels (ICON study) - preliminary results
Karen Pien a, Koen Putman b, Marie Luka De Deken b, Kurt Barbé b
Introduction
In March, Europe became the epicenter of COVID-19, exerting pressure to even the most resilient health care systems. Re-allocation of resources (personnel, units, material) was needed to provide an answer to the massive increase in infected patients, as well as to protect the care labor force and to save non-COVID-19 patients. This was in part achieved by postponement of non-urgent hospital appointments and procedures. Additionally, patients were minimizing their symptoms and avoided approaching health care facilities because of anxiety for infection. Prior epidemic outbreaks showed a large indirect impact on health care utilization due to such divergence of regular care.
The WHO recommends to focus not only on the burden of COVID-19 patients but also on the non-COVID-19 population. Our objective is to quantify the impact of the COVID-19 outbreak on hospital care of non-COVID-19 patients with the aim to render a more efficient healthcare planning as well as management during pandemic waves.
The goal of the project is four-folded:- To develop a prediction model to plan the need for ICU capacity, non-ICU capacity and rehabilitation beds for both COVID-19 and non-COVID-19 patients;
- To analyze the size of reduction in non-COVID-19 admissions during COVID-19 outbreak compared to the pre-pandemic situation for all DRG's;
- To analyze the differences in hospital length of stay, risk of mortality and severity of illness per DRG between pre-COVID-19 and during the pandemic period;
- To analyze the impact of the pandemic on the total amount of reimbursement per DRG between the pre-COVID-19 period and during the outbreak.
Methods
We performed a retrospective study, comparing admission and claims data for the period 2019, 2020 and 2021. In order to achieve the project goals, a dataset is constructed consisting of variables that are standardly registered in the Minimal Hospital Data (MHD) and claims data.
Results
The first aim to construct a time-series model for prediction of the bed capacity was examined. During the pandemic period such a time series behaves non-stationary due to strategic interventions as well as policy measures. In order to deal with the non-stationary external influences, we studied an Autoregressive-integrated-moving-average model with an exogenous input (ARIMAX).

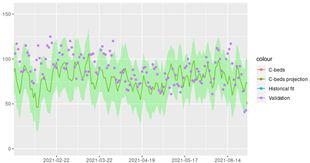
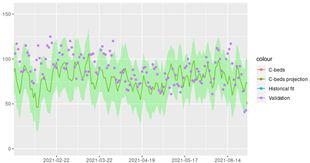
Figure 1: ARIMA time-series model for the first wave Surgical beds (C-beds)
In Figure 1 the ARIMAX modelling approach is illustrated on the surgical beds where the training period (left plot) and validation period (right plot) are shown. During the first pandemic wave, one can see the sudden down-scaling of surgeries which is repeated during the second wave in the fall. The model can describe this non-stationary behavior while understanding that this was an external influence. Nonetheless, the model is able to extrapolate this behavior to the next year resulting for the third wave though the model predicts a less abrupt drop which validates nicely to what was measured.
Conclusions
The model approach is promising to study and answer the different research questions stated. Indeed the model is a behavioral model which can fit the past as well as providing a reasonable prediction for the future while correcting and detecting the non-stationary interventions. Due to the applied model, its parameters allow proper interpretation to enhance future hospital planning.
a University Hospital Brussels, Belgium
b Free University Brussels, Belgium
Original Version in PDF